
There is no health without mental health
The World Health Organization constitution states: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Mental health is defined as a state of well-being in which every individual realizes their own potential, can cope with the normal stresses of life, can work productively and fruitfully and is able to make a contribution to their community.
Mental health is part of our overall health, and influences how we feel, think and behave. It is also interlinked with our physical health. Mental health is not just the absence of distress or illness, but includes a sense of well-being, maintaining supportive relationships and feeling that one can be meaningfully productive in the community and are able to cope with the typical stresses of life.
Mental health and mental health conditions exist on a continuum that most of us go up or down as we go through life and have both positive and adverse experiences.


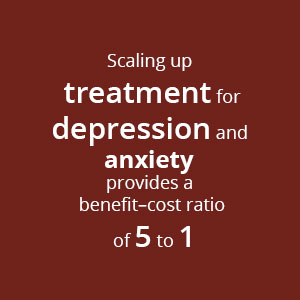
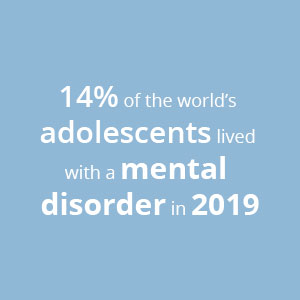
Latest statistics are in the recently released World Mental health report:

Every 40 seconds, a person dies by suicide somewhere in the world. It is the fourth leading cause of death for 15 to 29 year-olds world-wide. Every year, more than 700,000 people die by suicide, and for each person who dies by suicide, an additional twenty people are estimated to have attempted suicide. Suicidal thoughts and acts are often related to mental health conditions.
But suicides can be prevented.

What are common mental health conditions?
Some facts about mental health conditions. They…
There are five major types of symptoms of distress and mental health conditions:

Most people experience stressful situations and periods of time in their lives, that lead to varying levels of distress or even to the development of mental health conditions. Many factors influence how we are affected by stressful experiences, including the severity of the event or situation, previous experiences, our age, the level of threat we feel, how long the stressful situation lasts, the impact it has on our loved ones and our future, etc.
Some stressors are personal, whilst others are global and affect us all. The current Covid-19 pandemic, for example, has impacted mental health of people all over the world and especially that of young adults. Other common stressors that can affect mental health are facing poverty and not being able to meet basic needs, living in situations of conflict and uncertainty, and living in isolation.

People who experience adverse events or situations in childhood, such as neglect, abuse, exploitation, exclusion and violence are at high risk for experiencing distress or mental health conditions in childhood or later in life.

There are a few mental health conditions that are hereditary, but it is important to keep in mind that most mental health conditions are strongly influenced by environmental factors, so even if a parent has mental condition, it is not certain their children will also develop the same problems.

Malnutrition, especially in children and pregnant women can lead to physical, cognitive, motor and developmental problems for the child, that can all lead to the development of mental health conditions. Some medical problems (such as kidney or liver failure) or medicines (such as some used to treat high blood pressure) can sometimes lead to the development of mental health conditions. Brain infections, illnesses (including strokes) or injuries can lead to epilepsy, dementia and other mental health conditions.

There is stigma associated with mental health in every society. Stigma makes it difficult for a person with mental health conditions, and sometimes also for their family members, to talk openly about the problems or seek help when needed, as they may meet prejudice (negative attitude) or discrimination (negative behaviour) from those around them. Stigma often results from a lack of understanding of mental health conditions through a lack of information or misinformation.
Talking about mental health is important as many people have limited information about mental health and mental health conditions. It also helps to clarify incorrect myths that lead to stigma and discrimination. Breaking stigma and discrimination makes it easier for those who need help to ask for it.
Promote mental health and prevent the development or worsening of mental health conditions by focusing on healthy lifestyles, early childhood development, strengthening life skills and caregiving skills, suicide prevention, substance use prevention and self-care for community providers. See some useful resources from PS Centre on Life skills, Suicide Prevention and Self-care.
Provide support for people with mental health conditions involves promoting their human rights, learning to identify mental health conditions, engaging and building relationships with people living with mental health conditions, providing psychological interventions, referring for more care and services and providing support to careers and families.
UNICEF provide guidance for parents and caregivers on how to talk with children of different ages about mental health concerns: What’s on your mind? | UNICEF
There is a wide gap between people who could benefit from care and support for mental health conditions and those who are able to access appropriate social care and mental health services. This is referred to as the global mental health gap. An estimated two thirds of people affected by mental health conditions do not receive treatment, even in high-income countries.
In response to this, the World Health Organization (WHO) run a programme called the mental health Gap Action Programme (mhGAP) that seeks to address the lack of care for people suffering from mental, neurological and substance use (MNS) conditions. There are different strategies being used to address the mental health gap, and one of these is to promote and enable community mental health care.
Community mental health care is care in communities that:
Community platforms are ways of bringing health and social welfare services to people where they live and work. It can include multiple settings and a range of providers offering a spectrum of activities. Settings include health settings at or below the level of primary care (such as village health clinics or community outreach teams) and non-health settings such as neighbourhood and community groups, the social welfare sector, schools and workplaces.
Community providers range from community health workers, school nurses, teachers, police, social workers, youth workers, village elders, other community leaders, and members of the community including peers, families and friends of people living with mental health conditions.
The spectrum of activities and interventions that can be run as part of community mental health care cover the continuum of mental health and range from talking about mental health, mental health promotion and prevention of problems to support for people with mental health conditions and services for recovery and rehabilitation. Some activities are for the whole community whilst others target groups at higher risk of developing mental health conditions, or who are already experiencing such problems.
Promote recovery and rehabilitation for people with mental health conditions with community follow-ups, vocational, educational and housing support, social recovery and connectedness, self-management and peer support.
The Community-based Mental Health training manual provides guidance to programme managers and community providers on how to build the capacities of community health workers and volunteers by promoting and addressing mental health needs in their communities. With this training guide, the IFRC Psychosocial Reference Centre intends to promote the expansion across the Red Cross Red Crescent Movement of community mental health care services that go beyond primary health-care settings.
Communities play a vital role in
Specific considerations need to be taken in community mental health care when working with the following high-risk populations
Scalable psychological interventions are ones that can be offered to many more people than regular psychological treatments, and reach is therefore scaled up. People without a formal mental health professional qualification can be trained and supervised to deliver low-cost, low-intensity, scalable psychological interventions in a stepped care approach.

Why should we focus on mental health and psychosocial support in National Societies?
During armed conflict, natural disasters and health emergencies, the need for mental health and psychosocial support increases dramatically. Existing support systems are often strained.
What are the steps we should take in our National Societies if we want to work more with mental health?
Care in communities
IFRC are developing guidelines on how to design, implement and evaluate Care in Communities programmes. These programmes involve community and home-based care and support for physical and psychological well-being. The guidelines include a chapter on psychosocial support and community based mental health care.
Integrating mental health care into primary and community health care
Integrating mental health care in schools and primary & community health care has many benefits, including access to persons needing care, sites for providing care; it is often less stigmatising to access help at existing health care centres, social care service points and in schools; it is a good way to address shortages of staff and specialised services; it is cost-effective, and provides a good opportunity for advocacy, awareness and education on mental health.
What does this mean for psychosocial support activities and approaches? (Should National Societies now focus on MH and less on PSS?
No, there is as much need for psychosocial support activities as ever. In the RCRC movement we need to strive to achieve a continuum of care across the different layers of interventions. Adding focus on community mental health care in your work complements existing psychosocial support work, aiming to help those with more severe distress than usually targeted with psychosocial support. Psychosocial support activities that promote social connectedness are also part of community mental health care in promoting healthy living, supporting people living with mental health conditions, and promoting recovery and rehabilitation. The Red Cross Red Crescent work with MHPSS is guided by the Movement’s mental health and psychosocial support framework.
What can we do collectively to help improve mental health care in our own communities?
What can you do in your NS to include or improve focus on mental health care in your work?
Include or improve focus on mental health and psychosocial well-being in all integrated responses and programs (including budget allocations).
Build understanding and skills in mental health to prevent the development, and to respond to, severe distress or mental health conditions. Key activities are to train National Society staff and volunteers in Psychological First Aid.

Red Cross Red Crescent Movement MHPSS Hub
Hejrevej 30, st.
2400 Copenhagen NV
Denmark
Site language:
