
Using digital methods can help us reach more people and be more inclusive in the growing MHPSS area. The increased availability of Internet and mobile technologies coupled with the potential effectiveness of low-intensity psychological interventions provides opportunities to offer MHPSS services to a wide range of individuals.
Compared to face-to-face services, the spectrum of digital psychological and psychosocial support offers the following advantages:
Digital interventions prevent experiences of stigmatization and thus reduce barriers to seeking psychological and psychosocial help by enabling anonymous, non-public and secure use.
With digital interventions, MHPSS efforts can be diversified and larger parts of the population can be reached with fewer human and financial resources.
Digital interventions have the potential to improve access for geographically remote areas and can reduce barriers such as transportation costs, lack of free time, lack of childcare or fear of stigmatization.
With digital technologies broad-scale interventions that allow representation and community participation can be created. Content and design can be continuously adapted and contextualized to the needs of the target group with a participatory approach and be delivered to the users through appropriate channels. Once the technology is in place, the variable costs of digital interventions are low.
Over 300 studies from 20 years of research show, that technology-empowered and internet-based mental health services are an effective, resource-efficient extension of face-to-face approaches care.
Besides these advantages, there are, however, also critical aspects that need to be considered when choosing digital pathways to MHPSS:
Digital MHPSS services can differ according to the form of use, the extent and form of contact resp. in the degree of automation and the phase of the intervention.
– Psychoeducation about diseases and treatment options
– Forums
– E-mail
– Chat
– Phone/video call
– Prevention
– Self-help
– Treatment
– Aftercare
– Web-based self-help programs without contact to a professional or lay person (e.g. peer support)
– Short online contacts with a professional or a trained lay person
– Little contact compared to face-to-face services
– Support from professionals comparable to face-to-face services
– Require a similar amount of time as face-to-face services
– Communication can happen simultaneous/synchronous or delayed/ asynchronous
The MHPSS pyramid describes services on four different levels of specification. Digital services can be used on every level as e.g., digital self-care, focused support groups or technology-supported in-person treatments. It is important to determine at the beginning which target group with which needs is to be reached and to select the level of intervention accordingly.

The top layer of the pyramid includes specialized clinical care and treatment for individuals with chronic mental health conditions and for persons suffering such severe distress and over such a period of time that they have difficulty coping in their daily lives. Examples of activities include treatment centres for survivors of torture and alternative approaches to drug therapy. Services are provided within State healthcare and social welfare systems and in detention facilities.

The third layer of the pyramid includes prevention and treatment activities for individuals and families who present with more complicated psychological distress and for people at risk of developing mental health conditions. Examples of a ctivities include basic psychological interventions, such as counselling and psychotherapy, which are usually provided in healthcare facilities with accompanying outreach work in community facilities, where this is culturally appropriate.
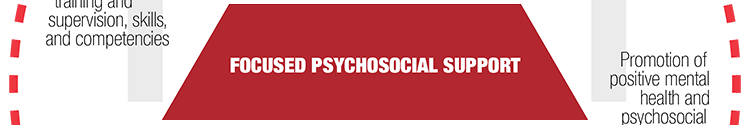
The second layer of the pyramid includes promotion of positive mental health and psychosocial wellbeing, and prevention activities, with a specific focus on groups, families, and individuals at risk. Examples of activities include peer support and group work. Focused psychosocial support can be provided by trained and supervised Red Cross Red Crescent staff and volunteers and/or trained community members.
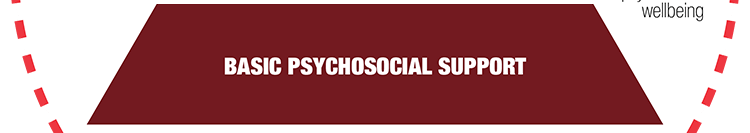
The first layer of the pyramid – promotes positive mental health and psychosocial wellbeing, resilience, social interaction and social cohesion activities within communities. Activities in this layer are often integrated into health, protection, and education sectors and should be accessible to 100% of the affected population, where possible. Examples of activities include psychological first aid (PFA) and recreational activities. Basic psychosocial support can be provided by trained Red Cross Red Crescent staff and volunteers and/or trained community members.
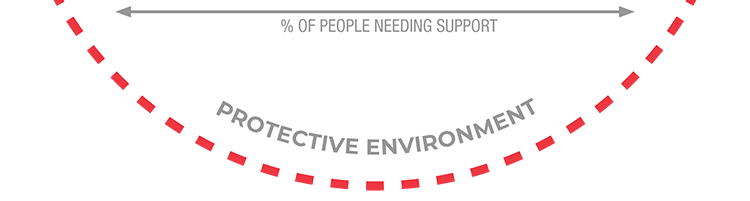
The outer circle around the pyramid includes promoting access to rights in accordance with International Laws, and upholding people’s dignity through providing “principled” assistance according to the seven fundamental principles of Red Cross Red Crescent Movement. Mental health and psychosocial support activities contribute towards protection outcomes; and similarly, protection activities contribute towards mental health and psychosocial support outcomes. Examples of activities include advocating for and ensuring people living with mental health conditions and psychological distress are enabled to access the necessary services and ensuring that people placed in detention facilities are treated respectfully.
Stay connected with psychosocial support and the latest news and events
The IFRC Psychosocial Centre (PS Centre) contributes knowledge and provides service to the Red Cross Red Crescent Movement. It assists in facilitating mental health and psychosocial support, promotes psychosocial wellbeing for affected groups, staff and volunteers, and increases awareness of psychological reactions in times of crisis or social disruption.
The PS Centre is hosted and supported by Danish Red Cross. It receives financial support from a number of National Societies, institutional and private donors including the European Commission and DANIDA.
© 2023 IFRC Psychosocial Centre. All rights reserved.
Site language: